Diagnosing Thyroid Disorders - What You Need to Know
Thyroid diseases are, arguably, among the commonest endocrine disorders worldwide. On a global scale, a staggering 200 million people have problems with their thyroid glands, with over 50 percent remaining undiagnosed. India too, has a significant burden of thyroid diseases. According to the latest study, it is estimated that about 42 million people in India suffer from Thyroid diseases, which account for approximately 21 percent of the global population.
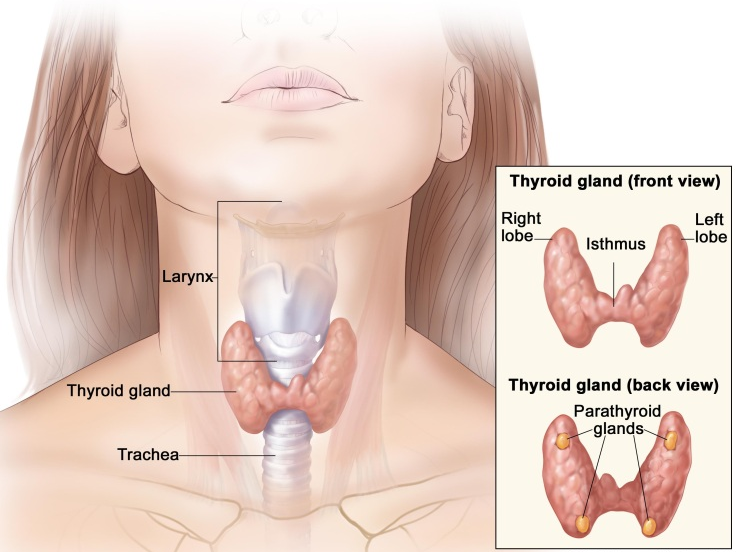
Being the largest endocrine gland in the human body, this butterfly-shaped, bi-lobed gland produces hormones which influence almost all the metabolic processes in the body. The thyroid gland produces two hormones, namely - Triiodothyronine (T3) and its precursor Thyroxine (T4). Under normal conditions, the thyroid produces T3 and T4 at a 20% - 80% ratio.
Thyroid-stimulating hormone (TSH) is another important hormone that is secreted by the anterior pituitary cells in the brain and its primary function is to increase the production of T3 and T4 by the thyroid gland.
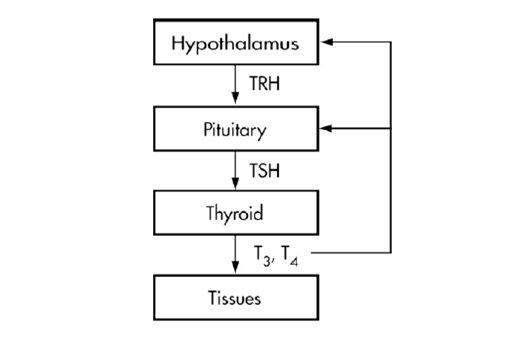 Fig 2: Control of thyroid hormone secretion (simplified).
Fig 2: Control of thyroid hormone secretion (simplified).
The five common thyroid diseases in India are:
- Hypothyroidism
- Hyperthyroidism
- Goiter and iodine deficiency disorders
- Hashimoto's Thyroiditis and
- Thyroid cancer
The two most common forms of thyroid disease are Hypothyroidism and Hyperthyroidism.
An under-production of thyroid hormones slows down the body’s metabolism, causing Hypothyroidism. Common symptoms of this condition are weight-gain despite eating sensibly, feeling cold, fatigue, depression, and possibly increased blood pressure and cholesterol levels.
Hyperthyroidism occurs when an excess of T3 and T4 speeds up the body’s metabolism and, if the mild condition is left untreated it can lead to complications such as severe weight loss despite a healthy appetite, nervousness, staring eyes, accelerated heart rate, and insomnia.
In both hypothyroidism and hyperthyroidism, there may be swelling of a part of the neck, which is also known as Goiter.
Table. 1 Clinical Reference Values of Thyroid Function Test
| Test |
Range |
| TSH |
0.5 - 4.7 mU/L |
| T3 |
0.92 - 2.78 nmol/L |
| FT3 |
0.22 - 6.78 pmol/L |
| T4 |
58 - 140 nmol/L |
| FT4 |
10.3 - 35 pmol/L |
Thyroid diseases are one of the silent epidemics of our time. They may get overlooked in the early stages because of their uncertain and ambiguous symptoms. However, Thyroid diseases are different from other diseases in terms of their ease of diagnosis, accessibility of medical treatment, and relative visibility in the form of a small swelling. Early diagnosis and treatment, therefore, remain the cornerstone of thyroid disease management.
The most useful marker of thyroid gland function is serum thyroid-stimulating hormone (TSH) levels. TSH levels are determined by a negative feedback system in which high levels of T3 and T4 suppress the production of TSH, and low levels of T3 and T4 increase the production of TSH. TSH levels are thus often used, as the first indicator of thyroid function.
- Elevated TSH levels can signify inadequate thyroid hormone production (hypothyroidism)
- Suppressed TSH levels can point to excessive thyroid hormone production (hyperthyroidism)
Table 2: Some Causes of Abnormal Serum TSH Concentrations
| TSH below normal |
TSH above normal |
|
|
|
- Pituitary/ hypothalamic disease with central hypothyrroidism (TSH unreliable)
|
- Pituitary thyrotroph adenoma; Pituitary resistance to thyroid hormone (central hyperthyroidism) TSH, unreliable
|
| |
- Generalized thyroid hormone resistance
|
- Prolonged thyrotroph cell suppression after recent hyperthyroidism in euthyroid or hypothyroid patient
|
- Thyrotoxicosis from overly rapid correction of severe hypothyroidism with parenteral T4
|
|
|
|
- Drugs, e.g. glucocorticoids, dopamine
|
|
- Problems with T4 treatment: Overdosage in treatment for fatigue or overweight, Altered gastrointestinal absorption because of drugs or disease, Altered T4 clearance because of drugs, Patient compliance problems, Prescription error, Testing too soon after T4 dose decrease
|
- Problems with T4 treatment: Underdosage based on misleadingly high total T4, Altered gastrointestinal absorption because of drugs or disease, Altered T4 clearance because of drugs, Patient compliance problems, Prescription error, Testing too soon after T4 dose increase
|
- Many severe systemic illnesses (Sick Enthyrid State)
|
- Recovery phase after severe systemic illness (Sick Enthyrid State)
|
- Combination of pulsatile TSH secretion and analytical precision limits
|
- Combination of pulsatile TSH secretion and analytical precision limits
Antibody in patient serum against antibody in TSH assay, causing analytical artifact
|
To further confirm the diagnosis, T3 and T4 levels in blood, are also measured, as a single abnormal TSH level can be misleading. When circulating in the body, T3 and T4 may be bound to transport proteins present in the blood. Only a small fraction of the circulating thyroid hormones are unbound or free, and thus biologically active. T3 and T4 levels can thus be measured as free T3 and free T4, or total T3 and total T4, which are the free hormones in addition to the protein-bound hormones.
Table 3: Combination of Results and their Interpretation
| T3 |
Low |
High |
High |
Normal |
| T4 |
Low |
High |
Normal |
Low |
| TSH |
High |
Low |
Low |
High |
| Condition |
Hypothyroidism |
Hyperthyroidism |
Hyperthyroidism |
Hypothyroidism |
Diagnosing thyroid disease is a process that incorporates a number of different types of examinations including clinical evaluation, blood tests, imaging tests, biopsies, and other tests, the most common and convenient being through laboratory tests for measuring the thyroid function markers – T3, T4, and TSH.
Immunoassays are not only the most common but also the most accurate and affordable methods for the quantitative determination of Thyroid function markers in serum/plasma.
Transasia’s range of ErbaLisa Thyroid ELISA kits for T3, T4, and TSH offers reliable solutions for Thyroid Disorder Diagnosis, for your laboratory.
References:
- Thyroid disorders in India: An epidemiological perspective. Ambika Gopalakrishnan Unnikrishnan, Usha V. Menon. Indian J Endocrinol Metab. 2011 Jul; 15(Suppl2): S78–S81.
- Laboratory Evaluation of Thyroid Function. Shashank R. Joshi. Supplement to JAPI, January 2011, Vol. 59, 14-20.
- https://en.wikipedia.org/wiki/Thyroid_disease.
- http://www.thyroid.org/wp-content/uploads/patients/brochures/FunctionTests_brochure.pdf.
- http://www.thyroid.org/thyroid-function-tests.
- https://en.wikipedia.org/wiki/Hashimoto's_thyroiditis