All You Need to Know about Malaria
Malaria remains a major global health problem, in-spite of the launch of several initiatives to eradicate it resulting in a decline in malaria-related morbidity and mortality. India currently accounts for 4% of the global Malaria burden and contributes 87% of the total Malaria cases in Southeast Asia.
The Malarial parasite is an obligate intra-erythrocytic protozoan of the genus Plasmodium. Humans can be infected with one (or more) of the four species of Plasmodia: namely, P.vivax, P.falciparum, P.ovale and P.malariae. Plasmodia are primarily transmitted by the bite of an infected female Anopheles mosquito, but infections can also occur through exposure to infected blood products (Transfusion Malaria) and by congenital transmission. Complications of Malaria are more common in pregnant women, babies, young children and older people.
Plasmodium – Life cycle & Morphology
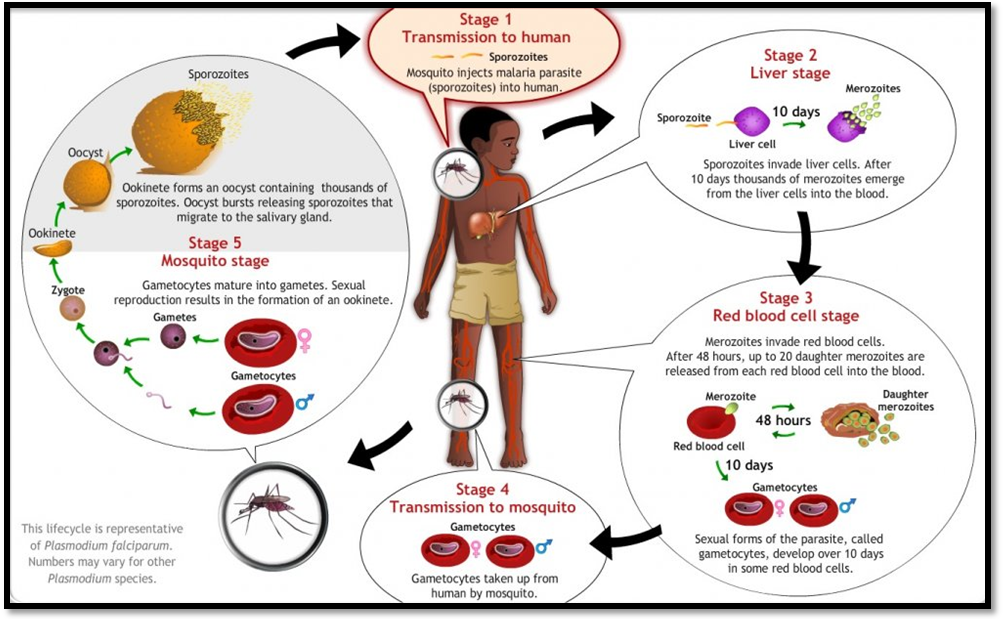
Plasmodia are transmitted by the female Anopheles mosquito. The life cycle of Plasmodium involves several distinct stages in the insect and vertebrate hosts.
- When the infected anopheles mosquito bites, the Plasmodium sporozoites are inoculated into the bloodstream
- Within an hour, sporozoites enter hepatocytes and begin to divide into exo-erythrocytic merozoites
- For P.vivax, dormant forms called hypnozoites typically remain quiescent in the liver; P.falciparum does not produce hypnozoites
- Once, merozoites leave the liver, they invade the erythrocytes, and develop into early trophozoites, which are ring-shaped, vacuolated and unnucleated
- Once the parasite begins to divide, the trophozoites are called schizonts, consisting of many daughter merozoites
- Eventually, the infected erythrocytes are lysed by the merozoites, which subsequently invade other erythrocytes
- The duration of each cycle in P.falciparum is about 48 hours
- After several cycles, some of the merozoites develop into gametocytes, the sexual stage of Plasmodia, which cause no symptoms in humans, but are infective for malaria.
Malaria Infection
Most people develop symptoms of falciparum malaria within 1 month of exposure; however, there have been reports of falciparum malaria presenting up to 4 years later. For non-falciparum malaria, the incubation period is usually longer; and P.vivax may even relapse, months or years after exposure due to the presence of hypnozoites in the liver. The longest reported incubation period for P.vivax is 30 years.
Complications of Malaria
Almost all severe forms and deaths from malaria are caused by P.falciparum. P.vivax rarely causes serious complications or death. Patients present with the clinical deterioration to severe malaria usually 3-7 days after fever onset. Severe malaria may also develop after initial treatment response and complete clearance of parasitemia due to delayed cytokine release. The major complications of severe malaria include the following:
- Cerebral Malaria – Clotting of the infected erythrocytes in the blood vessels in the brain. It is the most common clinical presentation and cause of death in adults, with severe malaria. Cerebral malaria is characterized by generalized convulsions, drowsiness and confusion, followed by coma lasting from several hours to days
- Pulmonary Edema – Buildup of fluid in lungs. Acute lung injury usually occurs a few days into the disease course. It may develop rapidly, even after initial response to anti-malarial treatment and clearance of parasitemia
- Renal failure – Acute renal failure in severe malaria may require temporary dialysis. Another renal complication – ‘Blackwater fever’ refers to passage of dark, red, brown or black urine due to massive intravascular hemolysis and resulting hemoglobinuria.
Diagnosis of Malaria
- Microscopy - Light microscopy of thick and thin stained blood smears, remains the standard method of diagnosing malaria. The level of parasitemia may be expressed either as a percentage of the parasitized erythrocytes or as the number of parasites per microliter of blood. However, the diagnostic accuracy of microscopy relies on the quality of the blood smear and experience of laboratory personnel.
In falciparum malaria, parasitized erythrocytes may be sequestered in tissue capillaries resulting in falsely absent/ low parasite count in the blood smear.
- Rapid Diagnostic Tests (RDTs) – Antigen-detecting malaria rapids are an important tool for fever case management and routine malaria surveillance. These rapid tests can detect and differentiate species-specific circulating parasite antigens, targeting either Histidine-rich protein-2 (HRP-2) of P.falciparum, Pan-species Lactate dehydrogenase (Pan pLDH); or parasite-specific Lactate dehydrogenase (eg. Pv-specific pLDH). The rapid tests drastically lower the TAT, have an acceptable sensitivity & specificity; and are suitable for limited resource setups. Antibody detection has no value in the diagnosis of acute malaria; hence it has been banned by the Indian government.
- Malaria Antigen ELISA - For blood donor settings in endemic areas, ELISA for the detection of Pan pLDH is ideal for screening multiple blood samples in a smaller time interval.
Transasia Bio-Medicals Ltd. offers both ELISA and rapid kits for detection of malaria. ErbaQik rapid tests for the detection of malaria, utilizes Black Gold Particle in the conjugate to create distinctly coloured bands, giving it a unique dual colour advantage. ErbaQik rapids are the only bi-colour detection rapid test in India, with enhanced sensitivity and specificity and, have been validated and approved by reputed NABL laboratories. ErbaLisa PAN (LDH) Malaria ELISA is another innovative tool for the Malaria screening in blood banks.

Every year, World Mosquito Day is observed on 20th August, to mark the historic discovery by Sir Ronald Ross, a British doctor, in 1897. He discovered that infected female Anopheles mosquitoes transmit the malaria parasite – Plasmodium, to humans. World Mosquito day is celebrated to create awareness about the threats and prevention of Malaria, spread by the world’s deadliest animal.
Transasia supports our nation’s aim to become malaria-free by 2030, by providing better options for early and accurate diagnosis of the disease.